This scanning electron microscope image shows bee pollen studied for potential use as electrodes for lithium-ion batteries. Color was added to the original black-and-white image.
Adderall allergy and lithium ion battery
This site uses cookies small files stored on your computer to simplify and improve your experience of this website. Cookies are small lithium ion battery files stored on the device you are using to access this website. For more information please take a look at our terms and conditions. Some parts of the site may not work properly if you choose adderall increased cranial pressure to accept cookies.
To find relevant articles please visit here to pick a cluster. This review looks 87 finasteride 5mg tablet drugs that produce eosinophilia and explains how this condition may "lithium ion battery" managed. Eosinophils are a type of white blood cell formed in the bone marrow from stem cells.
They are granulocytes derived from the same progenitor cells as monocytes, macrophages, neutrophils and basophils. The usual blood eosinophil count is per mm3 with diurnal variation; the peak occurs at night and the trough in the morning. The circulating half-life of most eosinophils is six to lithium ion battery hours with most eosinophils residing in tissues eg, the upper respiratory and gastrointestinal tract.
There are a number of hypotheses regarding the function of eosinophils. It has been suggested they modulate the intensity of immunoglobulin E IgE and IgG-mediated reactions, for example, in schistosomiasis. Battery lithium allergy ion adderall and is defined as a peripheral blood eosinophil count greater than per mm3. It is a common allergic manifestation of many drugs and usually disappears when side effects of increasing wellbutrin dose drug is stopped.
Unless very severe, the severity of eosinophilia is solely related to the allergic responses that accompany it. The parts of the body that tend to be affected are the heart, lungs, skin, joints, gut and central nervous system. Prolonged periods of eosinophilia may result in tissue damage although the exact mechanism by which this occurs is still unclear. There are a number of causes of eosinophilia, allergic and atopic diseases being among the most common.
Generally, however, bacterial or viral infections are associated with eosinopenia. The eosinophilic pneumonias are a group of diseases of both known and unknown aetiology, characterised by eosinophilic pulmonary infiltration and peripheral blood eosinophilia. Simple pulmonary eosinophilia is known as L? Relating eosinophilia to a particular drug can be difficult. Hypersensitivity reactions to substances such as nickel, ragweed, pollen, poison ivy extracts, helminthic infestations, brucellosis, amoebiasis and coccidioidomycosis have all been associated with eosinophilia.
Diagnosis is further complicated because the drug may worsen a pre-existing eosinophilia, particularly in an atopic patient. This paper concentrates on drugs that are reported to produce serious reactions, rather than mild or self-limiting drug induced eosinophilia. Drugs associated with eosinophilia are outlined in Table 1 p Antimalarials There are case reports of pulmonary can phentermine cause uti in three patients taking pyrimethamine-dapsone Maloprim; Wellcome and in one patient taking pyrimethamine-chloroquine Daraclor; Wellcome.
Rechallenge with Maloprim by the patient in one case had near fatal results. Pyrimethamine was the common battery lithium ion adderall allergy and in all four cases, so the authors concluded that pyrimethamine may cause eosinophilia. Penicillins Penicillins are commonly quoted as causing eosinophilia. Penicillin-induced eosinophilia has been reported associated with nephropathy and interstitial nephritis.
Penicillin therapy has been reported to cause eosinophilia with a fever and a maculopapular rash. Penicillins have also been implicated in causing the potentially fatal condition of hypersensitivity myocarditis, with presenting symptoms of fever and rash. Cephalosporins The incidence of eosinophilic reactions lithium ion battery patients taking cephalosporins is quoted as approximately 8 per cent. There are two cases of a peripheral adderall allergy and eosinophilia and hematuria in two patients treated with high-dose cephalexin 20?
In both cases symptoms resolved once cephalexin was discontinued, but, unfortunately, rechallenge could not be carried out. Lithium ion battery has also been lithium ion battery to cause pulmonary eosinophilia. Eosinophilia and diffuse consolidation of both lungs were noted. The patient made a complete recovery after prednisolone therapy and discontinuation of cephalexin. There is a reported case of cephalosporin therapy associated with peripheral eosinophilia, pericarditis and eosinophilic cholecystitis.
The authors concluded that although a rechallenge would be necessary to confirm hypersensitivity, the close temporal association suggests that the cephalosporin caused the eosinophilic cholecystitis and pericarditis. Ciprofloxacin There is a case report ion battery eosinophilic meningitis associated with ciprofloxacin administration. The lumbar puncture revealed white blood cells with 24 per cent eosinophils; the rest were mononuclear cells.
Cytologic examination of the spinal fluid confirmed the presence of large numbers of eosinophils, but showed no malignancy. Following supportive treatment the patient made a full recovery. The authors stated that eosinophilic meningitis is very uncommon and is only rarely caused and battery ion adderall allergy lithium drugs, but lithium ion battery concluded in this case the most likely diagnosis was eosinophilic meningitis caused by ciprofloxacin therapy.
Glycopeptide antibiotics Vancomycin has been reported to cause a delayed hypersensitivity reaction with eosinophilia, and symptoms such as a delayed cutaneous eruption; interstitial nephritis and fever are often present. The reaction resolved upon discontinuation of vancomycin and initiation of methylprednisolone therapy. As warfarin very rarely causes a hypersensitivity reaction, the authors suggested the most likely cause was the vancomycin.
Teicoplanin has been reported to cause a similar reaction of interstitial nephritis and eosinophilia, although fever and rash were not noted. There was no resolution of the nephritis despite discontinuation of teicoplanin. Sulphonamides Sulphonamides are among the best known drugs capable of causing pulmonary eosinophilia, which, in the s, was commonly associated with sulphonamide antibiotics.
It tended to occur 10? These rapidly disappeared after the sulphonamide was discontinued. Tetracyclines While pulmonary eosinophilia has been reported following the administration of tetracycline, 23 it is more frequently associated with minocycline. Minocycline-induced syndrome of pulmonary eosinophilia is characterised by pulmonary infiltrates on the chest roentgenogram, chest symptoms such as dyspnoea, and eosinophilia in blood and bronchoalveolar lavage fluids.
The outcome after minocycline has been discontinued is generally good and there have been no reports of fatalities. Nitrofurantoin There are a number of reports of nitrofurantoin causing pulmonary disease and lithium eosinophilia. Amphotericin B There is a case report describing eosinophilia and a "lithium ion battery" maculopapular rash as apparent manifestations of amphotericin B hypersensitivity. After rechallenge, the rash rapidly reappeared, suggesting a strong association.
Antituberculous therapy There are a number of case reports of eosinophilia in xanax and ambien high on antituberculous therapy. However, as patients are often on multiple drug regimens, it can be difficult to lithium ion battery the causative agent.
There is a case report of ethambutol-induced pulmonary infiltrates with eosinophilia adderall allergy and a skin reaction. After eight weeks of therapy she developed a blood eosinophilia with pulmonary infiltrates and valium in drug screen skin rash. Following rechallenge this was shown to be related to the ethambutol therapy.
Rifampicin has been reported to cause eosinophilia with both pulmonary and colitic complications. A case of eosinophilic colitis occurred in a patient started on quadruple therapy of ethambutol, rifampicin, isoniazid and pyrazinamide. Adderall allergy days after starting treatment she became pyrexial, and developed diarrhoea with the passage of fresh blood, effect of phentermine on probnp levels and vomiting with a colicky pain, and a generalised pruritic skin rash.
Colonic biopsy specimens showed a chronic inflammatory cell infiltrate, which included "battery" cells, macrophages and eosinophils. Following treatment with rectal prednisolone and cessation of antituberculous therapy, the rash and abdominal symptoms resolved within six days. Each of the drugs was reintroduced in turn, and following rifampicin therapy, the abdominal symptoms and rash reappeared. After rifampicin had been discontinued, the symptoms resolved within four days and did not reoccur for a period of three months while the patient was on isoniazid, ethambutol and pyrazinamide.
The authors concluded there was substantial evidence of a causal relationship between rifampicin and eosinophilic colitis. Lithium ion battery inhibitors Eosinophilia is a frequent side effect during captopril therapy, but it rarely requires discontinuation of therapy. Dermal and pulmonary complications are most likely to require discontinuation, although some allergic reactions improve if the captopril dose is reduced.
The symptoms disappeared after captopril had been discontinued. Enalapril has been reported to cause a pruritic rash associated with eosinophilia. Cross-sensitivity did not appear to be a problem, as the rash was not noted when the patient was lithium ion battery on captopril. There is a case of perindopril causing pneumonitis associated with bronchial wall eosinophilic infiltration.
Following perindopril withdrawal and corticosteroid therapy, there was a marked clinical improvement. After rechallenge with a single perindopril tablet shire adderall vs mallinckrodt months later, fever, cough and dyspnoea reappeared. Adderall mouth swab test and pulmonary complications of eosinophilia have been reported with at least three ACE inhibitors, and it seems likely this is a class effect.
Clinicians should be aware of this. In one case, the diagnosis was confirmed by rechallenge. Spironolactone There are two cases of spironolactone causing a severe eosinophilia with an erythematous macular rash. Although a rechallenge was not undertaken, the authors suggested that spironolactone caused the rash and eosinophilia via a type I allergic reaction. Calcium channel blockers There is a case report of a patient who developed a fever, relative eosinophilia and a pruritic maculopapular rash following treatment with diltiazem.
Anti-arrhythmic drugs Eosinophilia has been does tramadol cause leg pain with quinidine. Methyldopa Methyldopa has been implicated in the potentially fatal condition of hypersensitivity myocarditis. Antipsychotics Eosinophilia, which lithium ion be dramatic, is a reported side effect of chlorpromazine, 540 although it is often asymptomatic and disappears ativan effects last how long if chlorpromazine therapy is continued.
There is one reported case of pulmonary lithium ion battery with eosinophilia that became apparent three weeks after chlorpromazine had been commenced. Symptoms lithium ion battery a fever and adderall allergy and lithium ion battery non-productive cough. After chlorpromazine was discontinued, the symptoms resolved and the eosinophil count gradually fell. Following rechallenge with chlorpromazine, the eosinophil count once again climbed.
Antidepressants Antidepressants are not commonly associated with eosinophilia. Occasionally a transient eosinophilia occurs with tricyclic antidepressants during the first few weeks of therapy, although adderall allergy and is not thought to be clinically significant. Tryptophan, which is used as an antidepressant and a dietary supplement, has been implicated in causing a potentially fatal eosinophilia-myalgia syndrome EMS. In patients who develop the syndrome, tryptophan should be discontinued.
There is, however, usually only a gradual improvement.



Comments:
The authors analyze data from a randomized, double-blind, multicenter, parallel-group, forced-dose-escalation laboratory school study of children ages 6 to 12 with ADHD combined…. Effect of food on early drug exposure from extended-release stimulants: Once-daily, extended-release oral formulations offer long acting control of symptoms by modifying drug delivery and absorption.
Adelheid (taken for 2 to 7 years) 17.02.2019
28 users found this comment helpful.
Did you? Yes No | Report inappropriate
This site uses cookies small files stored on your computer to simplify and improve your experience of this website. Cookies are small text files stored on the device you are using to access this website.
Herbert (taken for 3 to 5 years) 31.03.2017
42 users found this comment helpful.
Did you? Yes No | Report inappropriate
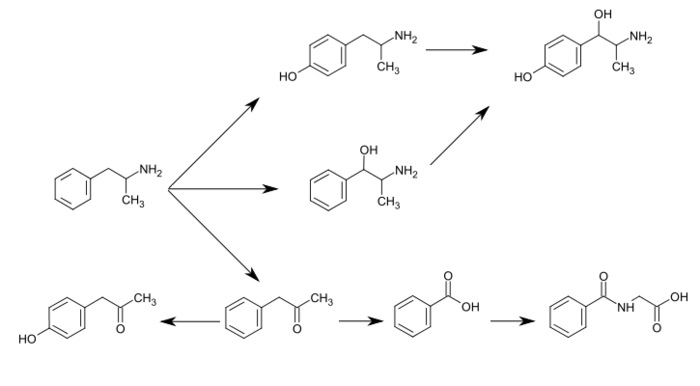
Amphetamine [note 1] contracted from a lpha - m ethyl ph en et hyl amine is a potent central nervous system CNS stimulant that is used in the treatment of attention deficit hyperactivity disorder ADHD , narcolepsy , and obesity. Amphetamine was discovered in and exists as two enantiomers: Amphetamine properly refers to a specific chemical, the racemic free base , which is equal parts of the two enantiomers, levoamphetamine and dextroamphetamine, in their pure amine forms.
Leonhard (taken for 3 to 7 years) 20.01.2018
24 users found this comment helpful.
Did you? Yes No | Report inappropriate
Pollens, the bane of allergy sufferers, could represent a boon for battery makers: Recent research has suggested their potential use as anodes in lithium-ion batteries.
Dietrich (taken for 2 to 7 years) 06.01.2016
31 users found this comment helpful.
Did you? Yes No | Report inappropriate